
As many as 3 in 4 patients with atrial fibrillation (AFib) have obstructive sleep apnea.1 While treatments such as continuous positive airway pressure (CPAP) can help maintain sinus rhythm after electrical cardioversion and improve catheter ablation success rates,2 screening and treatment for obstructive sleep apnea in patients with AFib remains poor.3 While at-home sleep apnea testing is a suitable alternative to in-lab nocturnal polysomnography,4 screening of this patient population is subpar. Fortunately, the VIRTUAL-SAFARI clinical study shows the WatchPAT® ONE at-home sleep apnea testing system can detect obstructive sleep apnea in patients with AFib using a completely remote management approach that patients find convenient, easy to use, and would recommend to others.5
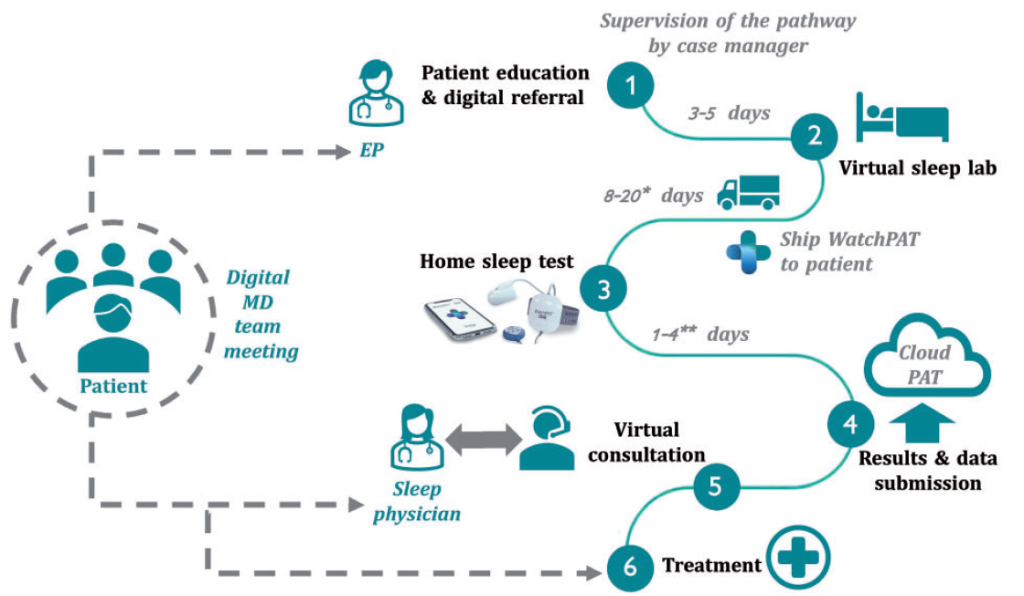
VIRTUAL-SAFARI management pathwayVIRTUAL-SAFARI researchers prospectively enrolled patients who had AFib requiring catheter ablation and without a prior diagnosis of sleep-disordered breathing (SDB) in the study. Patients had a teleconsultation with an electrophysiologist to discuss sleep-disordered breathing followed by a teleconsultation at a “virtual sleep lab.” Shortly thereafter, patients were shipped a disposable WatchPAT® device with paper and video instructions. Once patients wore the WatchPAT® device for 1 night of sleep—which occurred on average within 2 days of receiving the device (range 1-4 d)—the data was submitted to a secured cloud server and analyzed remotely by a sleep physician. If obstructive sleep apnea or other sleep-disordered breathing was diagnosed, the sleep physician generated a digital prescription in consultation with relevant providers and the patient so that the patient could begin in-home sleep apnea treatment.
Most patients with AFib had sleep-disordered breathing
During the VIRTUAL-SAFARI clinical study, 119 consecutive patients with AFib that were scheduled for catheter ablation underwent at-home sleep apnea testing. Eighty-five percent of patients in this cohort showed at least some degree of sleep-disordered breathing (ie, apnea-hypopnea index of 5 or greater).5 Moreover, 65 patients (55%) were diagnosed with moderate or severe sleep-disordered breathing that required treatment.5 Patients with moderate or severe sleep-disordered breathing diagnosis had significantly higher body mass indices (BMIs) than those with mild or no sleep-disordered breathing (BMI 29 ± 3.3 vs 27 ± 4.4 kg/m2; P<0.01). Researchers also determined that those with moderate or severe sleep-disordered breathing had higher thromboembolic risk assessed via CHA2DS2-VASc score (median 2 [1-3] vs 1 [12]; P=0.02)). Patients in this cohort predominately had obstructive sleep apnea patterns with little contribution from central sleep apnea.5
A remote, multidisciplinary, patient-centered approach to treatment
At-home sleep study data were analyzed remotely by a sleep physician, and in consultation with the patient’s electrophysiologist, the patient’s primary care provider, and the patient, a management plan was created. Positive airway pressure treatment was chosen by the multidisciplinary team for 25% of patients, a sleep position trainer was recommended for 5%, a mandibular repositioning appliance was recommended for 15% of patients, and more than 1 device/intervention was selected by 14% of patients. Patients without sleep-disordered breathing did not receive any direct sleep apnea treatment but were instead followed by their cardiologists and primary care physicians.
Patients report WatchPAT® ONE is convenient and easy to use
A critical barrier to any sleep apnea testing method is patient perception. If a testing method is not convenient, patients will not use it. Consequently, VIRTUAL-SAFARI study researchers conducted a patient satisfaction survey to determine if WatchPAT® ONE would be useful in real-world settings. VIRTUAL-SAFARI results showed5:
- 95% of patients agreed or strongly agreed with the statement: I liked being able to complete the SDB test at home, instead of in a sleep center
- 91% of patients agreed or strongly agreed with the statement: Using the WatchPAT® ONE was easy
- 86% of patients agreed or strongly agreed with the statement: I would recommend using the WatchPAT® ONE for SDB testing in the AFib clinic in the future
- 95% of patients agreed or strongly agreed with the statement: The instruction, consisting of the manual and the video, was helpful
The ease-of-use results agreed with recorded data during the study; only 6 patients (5%) had problems with obtaining proper recordings. In 4 of the 6 cases, WatchPAT® recordings were successfully obtained on a future night and only 2 patients required in-lab polysomnography.5
The VIRTUAL-SAFARI study: implications for cardiology practice
The clinical study results clearly show that fully remote sleep apnea testing is feasible for older patients with AFib (mean age 65 ± 9.5 y).5 Because treatment guidelines recommend in-lab or at-home sleep apnea screening for all patients with AFib, WatchPAT® ONE provides a completely virtual management pathway that is convenient for patients and providers. Cardiac electrophysiologists need only to add 1 referral and 1 treatment discussion to their catheter ablation workflows. VIRTUAL-SAFARI showed that patients scheduled for ablation procedures found WatchPAT® ONE was easy to use and recommended the virtual sleep apnea pathway to others. This approach promises to improve the detection and treatment of sleep-disordered breathing and, in turn, increase time in sinus rhythm and improve catheter ablation success rates for patients with AFib.
References
1. Stevenson IH, Teichtahl H, Cunnington D, Ciavarella S, Gordon I, Kalman JM. Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J. 2008;29(13):1662-1669. doi: 10.1093/eurheartj/ehn214
2. Linz D, McEvoy RD, Cowie MR, et al. Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol. 2018;3(6):532-540. doi: 10.1001/jamacardio.2018.0095
3. Khan A, Patel J, Sharma D, Riaz S, Demissie S, Szerszen A. Obstructive sleep apnea screening in patients with atrial fibrillation: missed opportunities for early diagnosis. J Clin Med Res. 2019;11(1):21-25. doi: 10.14740/jocmr3635
4. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479-504. doi: 10.5664/jcsm.6506
5. Verhaert DVM, Betz K, Gawalko M, et al. A VIRTUAL sleep apnoea management pathway for the work-up of atrial fibrillation patients in a digital remote infrastructure: VIRTUAL-SAFARI. Europace. 2021. doi: 10.1093/europace/euab229
