By Gilad Glick
To some it may come as a surprise that SDB (Sleep Disordered Breathing) or Sleep Apnea is common among AFIB patients, and that it has been found an independent major risk factor, significantly affecting outcomes.
However, leading electrophysiologists and cardiologists have already been increasingly aware of the link between Atrial Fibrillation and Sleep Apnea. Such clinicians seek to actively diagnose OSA and integrate effective screening tools to identify Sleep Apnea risk among their patients as part of their patient care pathway. In addition, the ESC and ACC have updated their AFib guidelines to include sleep apnea screening and treatment in consideration of accumulating evidence linking the two
Here’s a brief overview of the AFIB practice guidelines and evidence related to the link between sleep apnea and AFIB.
Clinical Practice Guidelines
According to the 2016 ESC guidelines for the management of atrial fibrillation interrogation for clinical signs of obstructive sleep apnea (OSA) in all AFib patients is a Class IIa, level B recommendation. Further, once OSA is diagnosed, treatment should be optimized to improve AF treatment results in appropriate patients (Class IIa, level B).1
These guidelines have recently been cited by the ACC.
The Heart Rhythm Society also published a patient brochure to educate AFib patients about Sleep Apnea symptoms and the importance of getting tested for sleep apnea and treating it to improve their overall health. You can find it here2.
The link between Atrial Fibrillation and Sleep Apnea
Obstructive Sleep Apnea is a known risk factor associated with both onset and recurrence of AFib after therapy. Sleep Apnea is now established as an independent predictor of AFib with a HR of 2.18.8
How common is Sleep Apnea among AFib patients?
In the general population, OSA (Obstructive Sleep Apnea) affects approximately 24% of men and 9% of women, between 30 and 60 years of age. The prevalence of Sleep Apnea rises with age. Up to 80% remain undiagnosed.2,3
Among AFib patients, the comorbidity of Sleep Apnea is estimated at about 49%.4,5 A recent study in Sweden showed a prevalence of over 80 percent of sleep apnea among patients treated for atrial fibrillation.
Mehra and colleagues showed, with a large, prospective, community-based cohort, that individuals with Sleep apnea had 4 times the odds to develop AFib as those without SDB (OR 4.02, 95% CI 1.03- 15.74) after adjustment for age, sex, BMI and prevalent coronary heart disease.6
How does Sleep Apnea and its management affect AFib outcomes?
A major challenge for electrophysiologists nowadays is a persistently high 1-year AFib recurrence despite treatment by cardioversion, catheter ablation or drugs. Often a repeat ablation is necessary to treat AFib efficiently, and AFib may still recur despite these additional interventions. Electrophysiologists were concerned about a group of patients who seemed refractory to maintenance of sinus rhythm despite aggressive therapy.
In recent years, multiple published studies linked untreated sleep apnea with substantial increases in the rate of AFIB recurrence – practically telling us that the common 20% – 40% recurrence rate has two groups: those with Sleep Apnea, about half the patients, with a much higher rate of AFib recurrence and the other half, without Sleep Apnea, with lower rate.
Moreover, when patients with confirmed OSA complied properly with CPAP Sleep Apnea treatment, ablation success rates improved to match those among non-apnea sufferers in all AFib types.
Sleep Apnea Treatment – what is the effect on AFib outcomes?
The first to show that treatment of Sleep Apnea correlated with a lower incidence of atrial fibrillation recurrence was the team led by Dr. Virend Somers4.
As far back as 2010, a group led by Dr. Andrea Natale, showed that Sleep Apnea was an independent predictor for PVAI failure, and that treatment with CPAP improved PVAI success rates. Patients not treated with CPAP in addition to having higher prevalence of non-PV triggers were 8 times more likely to fail ablation.7
A broader landmark study was published by Dr. Fein, Dr. Anter and colleagues. These authors found that AFib-free survival rate among patients with CPAP-treated OSA was similar to a group of patients without OSA (71.9% vs. 36.7%; p = 0.01). AFib recurrence following PVI in CPAP-nonuser patients was significantly higher (HR: 2.4, p < 0.02) and similar to that of OSA patients managed medically without ablation (HR: 2.1, p = 0.68). Summary of the study conclusions is below.8
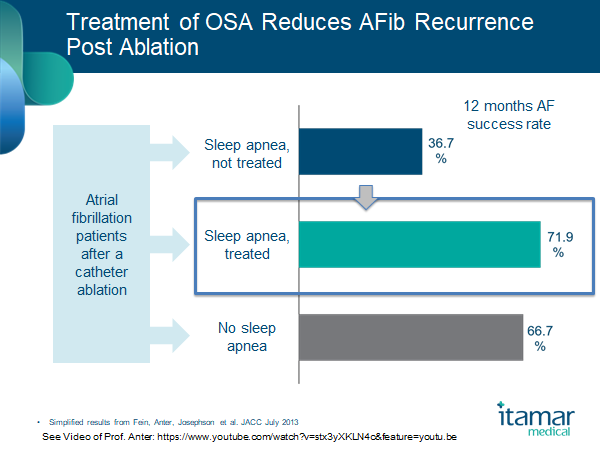
The authors concluded that CPAP is an important therapy in OSA patients undergoing RF Ablation that improves arrhythmia free survival. RF Ablation offers limited value to OSA patients not treated with CPAP.8
A recent study from Duke University found that patients who underwent focal impulse and rotor modulation (FIRM) ablation and also suffered from OSA, exhibited increased rotor prevalence, driven predominantly by an increase in RA rotors. CPAP therapy was associated with fewer RA rotors.10
Finally, a meta-analysis conducted by Dr. Shukla, Dr. Chinitz and colleagues from the Charney Division of Cardiology, New York University Langone Medical Center in NYC, found that the association between CPAP and reduced AF recurrence remained the same whether treated medically or with catheter ablation.9
CPAP use in patients with OSA was associated with a reduced relative risk of AF recurrence in comparison to non-users – with a 42% relative risk reduction and a very highly significant statistical data. Authors noted that the effect remained consistent and similar across patient populations irrespective of whether they undergo PVI.9
Clinical practice: Implementing AFib guidelines related to Sleep
Cardiologists are becoming increasingly aware of the possibility of the benefits of home sleep testing and cloud technology to connect with sleep specialists and pulmonologists and conduct wide screening for undiagnosed sleep breathing disorders, refer for treatment and follow up on therapy and CVD outcomes.
Given the strength of evidence, it’s no surprise that electrophysiologists were the first to take practical steps in integrating sleep medicine in cardiology care.
Since we started offering the WatchPAT home sleep test to cardiology departments around the world, we hear from physicians that they no longer convince their patients to take the test. The patients are eager to get tested at home as the process is so simple and cardiologists explain how essential it is to improve outcomes and AFib recurrence. The WatchPAT home sleep test is as easy for patients to use as a home holter monitor and clinicians can view the report via the cloud and share with pulmonologists to obtain interpretation.
And because cardiologists were anxious to verify that patients comply with treatment and linked non-usage to recurrence of AFib, we started connecting them with leading service and CPAP providers. We now offer customized solutions to all types of institutions or clinics, depending on size, workflow and physician needs.
To learn more about sleep and arrhythmias – we recommend this video series of the scientific symposium we sponsored at HRS in 2016.
I invite you to join learn more about Cardio Sleep solutions here.
References:
1 2016 ESC Guidelines for the Management of Atrial Fibrillation Developed in Collaboration With EACTS. Eur Heart J 2016; Aug 27:[Epub ahead of print]
2 http://resources.hrsonline.org/pdf/patient/HRS_AF_SleepApnea_R3.pdf
3 Young et al. The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults. N Engl J Med 1993; 328:1230-1235
4 Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation 2004; 110:364–7. [PubMed]
5 Seet & Chung, Anestsiology Clin 2010
6 Mehra R, Sleep apnea ABCs: airway, breathing, circulation, Cleve Clin J Med 2014;81:479–89 | Pubmed
7 Dimpi Patel el al “Safety and Efficacy of Pulmonary Vein Antral Isolation in Patients With Obstructive Sleep Apnea” Circulation Arrhy and Electro, 2010
8 Fein AS, Anter E., et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013; 62:300-305. | Pubmed
9 Shukla et al. CPAP Use on Recurrence of AF in Patients with OSA JACC: CLINICAL ELECTROPHYSIOLOGY VOL. 1, NO. 1-2, 2015
10 Friedman et al, Obstructive sleep apnea is associated with increased rotor burden in patients undergoing focal impulse and rotor modification guided atrial fibrillation ablation, Europace, eux248, https://doi.org/10.1093/europace/eux248
