By Efrat Magidov

Heart failure (HF) is a chronic, progressive condition in which the heart muscle is weakened and cannot pump enough blood to meet the body’s needs for blood and oxygen. Common symptoms include shortness of breath, coughing, excessive tiredness and leg swelling. In spite of continuous improvement of pharmacological and device therapy, HF remains a major public health problem associated with high morbidity, frequent hospitalizations and readmissions and high economical cost. Therefore, a better understanding of HF’s pathogenesis and co-morbidities is essential for improvement of risk stratification and prevention.
Among multiple co-morbidities, sleep-disordered breathing (SDB) and in particular obstructive sleep apnea (OSA), is the most common; Almost 50% of patients with HF have alterations of ventilation during sleep that can disrupt the positive effects of physiological sleep on the cardiovascular system. In two studies including patients with HF undergoing polysomnography, OSA was detected in 37% and 11% of patients, and the Sleep Heart Health Study – a perspective study comprising 6,424 men and women, indicated that the presence of OSA (defined as an apnoea–hypopnoea index (AHI) ≥10 per hour) favored the appearance of HF independently of other known risk factors, with a 2.20 relative risk.
The complex interaction between HF and OSA seems to be bi-directional; Some factors of HF can favor the collapse of the upper airways and thus increase risk of OSA. For example, HF is characterized by fluid shifts from the legs to central structures (peripheral oedema), especially in supine position, which can lead to upper airways narrowing. Conversely, OSA increase the risk of HF by multiple mechanisms; Obstructive apneas during sleep induce a series of systemic hemodynamic, autonomic, and humoral changes with adverse consequences for the cardiovascular system in individuals with normal ventricular function. The repeated occurrence of apneas and hypopneas has been associated with deranged endothelial function, an increase in the plasma concentration of inflammatory markers, increased platelet agreeability, and increased variability in blood pressure and heart rate.
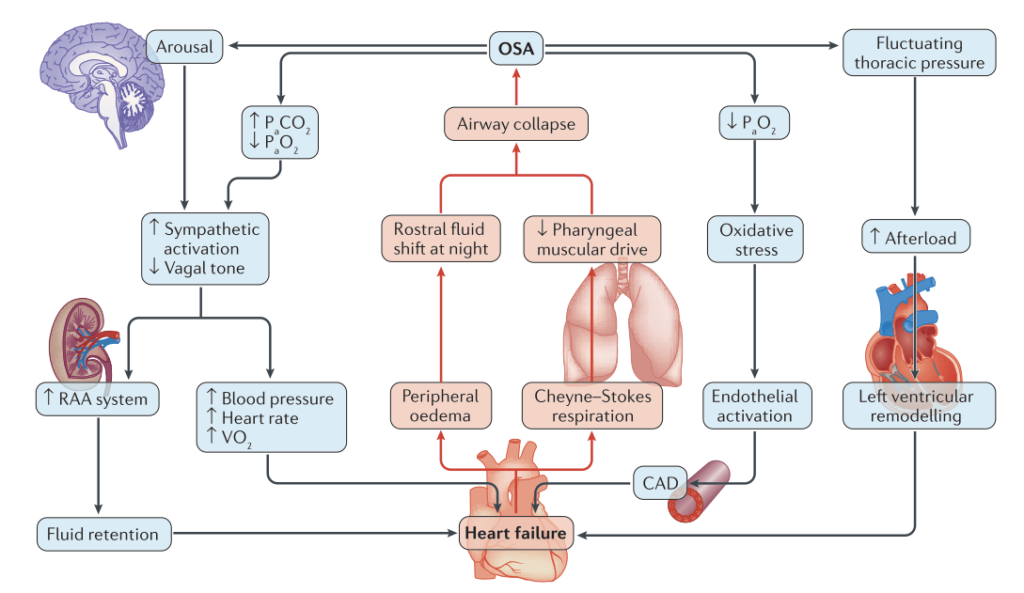
Moreover, the negative intrathoracic pressure during obstructive apnea results in increased venous return to the right ventricle and increased left ventricular (LV) transmural pressure, both are damaging the LV function. These recurrent events that accompany repeated obstructive apnea determine a further increase of the already elevated sympathetic activity in patients with HF, documented by increased plasma catecholamine. Obstructive events during sleep can also have long-term effects, for example by the induction of genes involved in ventricular remodeling caused by the repetitive increases in wall stress, and by inducing myocyte slippage and contractile dysfunction. Thus there’s a growing understanding that the OSA-HF interaction has causal aspects, and does not reflect mere co-morbidity.
Thus successful diagnosis and treatment of OSA is key for HF relief. In the first study to examine the effects of treating OSA in patients with HF, CPAP treatment was associated with a significant increase in mean LV ejection fraction and a reduction in HF related dyspnoea (shortness of breath). In a study led by the renowned cardiologist Gregory Lip, treatment of OSA by CPAP therapy significantly improved structural and functional changes in the LV. In the long run OSA treatment has also been shown to lower hospital readmission rate and mortality of patients with HF. Diagnosis is not always easy since most patients with HF and OSA do not complain of daytime sleepiness (the most pronounced OSA symptom), probably because of the high sympathetic tone in HF. Thus the occurrence of sleep-disordered breathing might not be identified unless a patient’s bed partner is also interviewed. The current recommendation for physicians is to test for OSA in patients with HF presenting with paroxysmal or recurrent atrial fibrillation, hypertension refractory to optimal HF therapy, increased body mass index and unanticipated pulmonary hypertension or right ventricular dysfunction.
Since attended polysomnography is a complex test that is expensive and not easily available, home sleep apnea test might be the best solution for these patients.
Sources:
- Butt, M., Dwivedi, G., Shantsila, A., Khair, O. A., & Lip, G. Y. (2012). Left ventricular systolic and diastolic function in obstructive sleep apnea. Circ Heart Fail, 5, 226-233.
- Kasai, T. (2012). Sleep apnea and heart failure. Journal of cardiology, 60(2), 78-85.
- Parati, G., Lombardi, C., Castagna, F., Mattaliano, P., Filardi, P. P., & Agostoni, P. (2016). Heart failure and sleep disorders. Nature reviews Cardiology, 13(7), 389.
