By Efrat Magidov

Sudden cardiac death (SCD) is defined as an “unexpected natural death from a cardiac cause within a short time period, generally ≤1 hour from the onset of symptoms, in a person without any prior condition
that would appear fatal”1.
In most cases SCD results from a malfunction of the heart electrical system, causing a sudden loss of heart function (sudden cardiac arrest). Without organized electrical input to the heart, there is no consistent constriction of the ventricles which manifests in an irregular rhythm (arrhythmia) and an inadequate cardiac output. Loss of consciousness shortly follows due to lack of blood flow to the brain, and unless emergency treatment is given immediately death is inevitable.
Although SCD is one of the largest causes of natural death, accounting for up to 450,000 deaths annually in the US2, strategies for risk stratification and prevention are still far from ideal. This is mainly due to the fact that SCD mostly occurs in people without any diagnosed cardiac problems, and thus an adequate characterization of risk factors is highly essential.

Such risk factor, that was poorly identified until recently, is obstructive sleep apnea (OSA).
The biological plausibility for OSA as a risk factor for arrhythmogenesis stems from its interventions with all three mechanisms of arrhythmias:
- Increased automaticity – triggered by the hypoxemia and respiratory acidosis accompanying the apneic event.
- Triggered activity – the enhanced sympathetic activity following an obstructive event can alter the afterhyperpolarization timing of the heart pacemaker cells.
- Reentry – respiration against a partially occluded airway results in a vagal stimulation which in turn can initiate a premature cardiac action potential and negative intrathoracic pressure is believed to cause micro scaring in the heart tissue as well.
In line with such important observations on the potential relationship between these two phenomena, a growing number of studies is trying to assess risk of SCD in OSA patients. One such attempt, and perhaps the most extensive one, was led by Dr. Virend Somers, the director of the Cardiovascular Facility and the Sleep Facility within Mayo Clinic’s Center for Clinical and Translational Science in Rochester, Minnesota.
In this 15 years controlled longitudinal study, 10,701 adults with suspected sleep disordered breathing admitted to the Mayo Clinic Sleep Disorders Center for a full night evaluation, the polysomnography over-night test. The apnea-hypopnea index (AHI) was calculated as the number of apneas/hypopneas per hour of sleep, and OSA diagnosis was established for an AHI 5 in accordance with AASM criteria.
The collection of follow-up data occurred up to 15 years (mean 5.3 years) from data of polysomnography to the date of SCD, resuscitated SCD, death from other causes or last follow-up. SCD was established when the cause of death was sudden cardiac death, (fatal) cardiac dysrhythmia, (fatal) cardiac arrhythmia, cardiac arrest, cardiorespiratory arrest; or coronary heart disease or myocardial infarction when the time interval from symptoms to death was specified ≤ 1 hour. Overall, 142 patients had resuscitated or had a fatal SCD, representing an annual rate of 0.27% for the study population.
In accordance with the researchers’ hypothesis, the presence of OSA predicted incident SCD and the magnitude of risk (hazard rate, HR) was predicted by multiple parameters that characterize OSA severity, including the AHI and nocturnal hypoxemia (AHI>20: HR 1.60; mean O2sat<93%: HR 2.93; lowest O2sat<78%: HR 2.60, all p<0.0001, Figure 1).
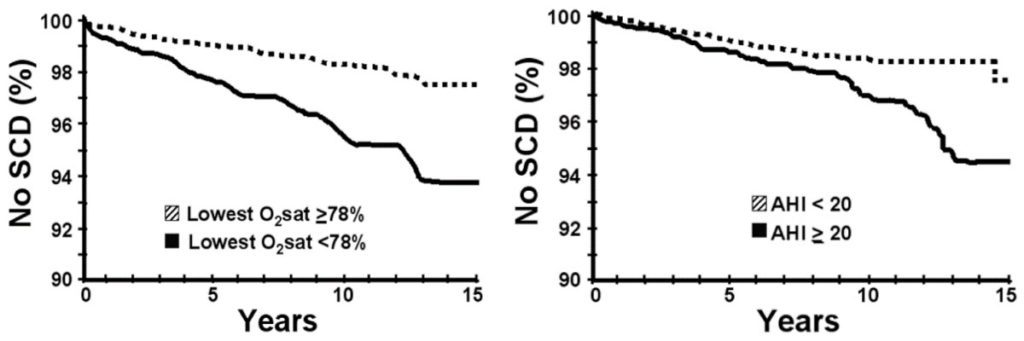
Figure 1
These findings are in line with previous studies demonstrating a two-to-fourfold greater risk of abnormal heart rhythms in people with OSA than people without OSA3-4. This risk had been shown to disappear completely in patients with treated OSA5. Taken together these findings stretch the importance of OSA diagnosis and treatment in SCD risk reduction.
WatchPAT, Home Sleep Apnea Test device, is an easy to use, effective and accurate tool for OSA diagnosis. You may learn more about WatchPAT and our comprehensive “Total Sleep Solution” for Cardiology practices in www.cardiosleepsolutions.com
- Zipes, D. P., & Wellens, H. J. (1998). Sudden cardiac death. Circulation, 98(21), 2334-2351.
- Kong, M. H., Fonarow, G. C., Peterson, E. D., Curtis, A. B., Hernandez, A. F., Sanders, G. D., … & Al-Khatib, S. M. (2011). Systematic review of the incidence of sudden cardiac death in the United States. Journal of the American College of Cardiology, 57(7), 794-801.
- Mehra, R., Benjamin, E. J., Shahar, E., Gottlieb, D. J., Nawabit, R., Kirchner, H. L., … & Redline, S. (2006). Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. American journal of respiratory and critical care medicine, 173(8), 910-916.
- Gami, A. S., Howard, D. E., Olson, E. J., & Somers, V. K. (2005). Day–night pattern of sudden death in obstructive sleep apnea. New England Journal of Medicine, 352(12), 1206-1214.
- Doherty, L. S., Kiely, J. L., Swan, V., & McNicholas, W. T. (2005). Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest, 127(6), 2076-2084.
